CPS Manifesto 2026: Transforming Scotland's Health through Detect
Published: 06/11/25
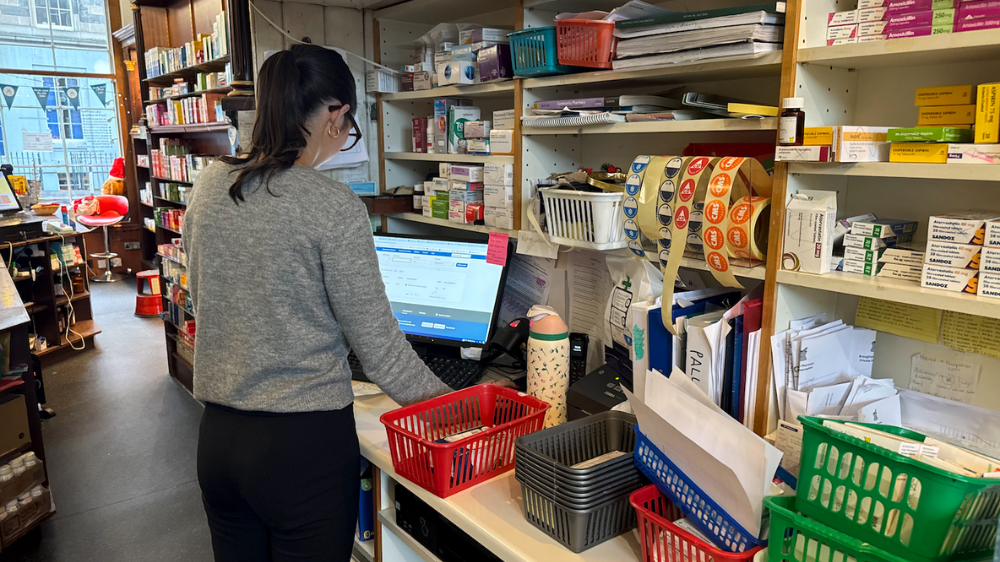
Community Pharmacy Scotland (CPS) recently attended the Transforming Scotland's Health 2025 event at Dynamic Earth, Edinburgh. Policy Officers Gill Paterson and Gordon Winter were in attendance, focusing on highlighting the role of community pharmacy in preventing, detecting, and treating ill health.
We heard from a range of speakers, from Dr Charlotte Refsum to the Cabinet Secretary for Health and Social Care, Neil Gray. A clear theme ran through all areas of health and social care in Scotland: a focus on early detection, greater investment in prevention, and, crucially, improvements in infrastructure through the use of new and emerging technologies to support these developments.
Our recently released 2026 Manifesto echoes a lot of what has been spoken about at the event. All areas of Health & Social Care are striving for these improvement, however at CPS we believe community pharmacy is particularly well placed to deliver them. One of the key focuses of our 2026 Manifesto is that of detecting ill health in those who may present at the Community Pharmacy with or without symptoms. This allows earlier interventions and lifestyle advice, potentially reducing critical health events that could have been prevented through screening, for example, heart attacks and strokes. Thanks to advances in medicines and strategies to tackle cardiovascular risks across the population, the death rates of heart and circulatory diseases have declined over the last several decades. However, despite this significant improvement, an estimated 700,000 people in Scotland are living with a cardiovascular disease today and this collection of conditions still cause 29% of all deaths.
Thankfully, the main predictive factors for heart attack and stroke are well established and easily measured:
high blood pressure
high cholesterol
atrial fibrillation *
Like many other diseases, the burden of cardiovascular disease is distributed disproportionately, with those in areas of multiple deprivation having higher blood pressure and cholesterol levels than their counterparts in more affluent areas. As these predictive factors can go completely unnoticed in terms of symptoms, many people in Scotland have no idea that their risk of developing or already having cardiovascular disease is high. Crucially, this means that they often have no reason to be routinely engaged with NHS services, so are never screened despite other risk factors such as age and weight suggesting that they should be.
It has already been recognised in several countries that the reach of pharmacies into communities - particularly in more deprived areas - presents an opportunity to engage with and screen people who would otherwise not present to the health service until they experienced symptoms or a cardiovascular event.
NHS England has since 2021 commissioned an opt-in hypertension case-finding service which sees pharmacy team proactively offering targeted blood pressure checks - consistently testing over 200,000 patients each month of late. Beyond case-finding and referrals, the community pharmacy network in Scotland’s prescribing capability opens up possibilities around initiation of therapy where appropriate. Although the UK National Screening Committee does not currently recommend that a standalone national Atrial Fibrillation screening programme is established, many modern blood pressure devices are designed to pick up on heart rate and rhythm irregularities, which would further support the wider cardiovascular detection agenda if used in such a scheme. Given the successes of the service in England, and similar projects across Europe, CPS believes that the community pharmacy network should be commissioned to undertake cardiovascular screening which may involve measurement of these predictive factors in target populations.
We believe that NHS and Scottish Government public health experts should work with CPS to identify screening programmes that the community pharmacy network can support and add value to.
One other area is targeted diabetes screening. The NHS in Scotland spends around £875 million (4.5% of the total budget) annually on diabetes care for almost 340,000 people living with the disease. Over half of this is spent on managing avoidable diabetes-related complications, which are more than twice as likely to occur in people from areas of multiple deprivation. Diagnoses have more than doubled in the last 20 years.
Whilst the ideal scenario would be to prevent diabetes, we should also strive to detect cases of diabetes as early as possible. This can be a challenge as often those unknowingly living with the disease or even the risk of developing it have no reason to engage proactively with the health service.
As such, reaching out into communities with targeted and evidence-based screening programmes should form part of the efforts to reform the NHS – and we believe that the community pharmacy network is ideally placed to support this shift in approach. A recent study using community pharmacy teams in NHS Tayside to identify at-risk individuals and take them through an assessment (and if necessary a point-of-care blood test) has shown that this approach is not only feasible, but more effective than traditional services in terms of use of resources and patient acceptability.
In this study,
46% of those approached to undertake the risk assessment were identified as being at moderate/high risk of developing diabetes. This cohort of people, who would otherwise be unaware of their risk of developing diabetes, were then supported to access advice and care appropriate to their blood test results.
87% were signed up to a digital lifestyle education app,
6.2% met the criteria to be referred to an intensive 9-month diabetes prevention programme.
6.3% were referred to their GP under suspicion of undiagnosed disease.
Whilst these results are in themselves indicative of success, there is huge potential for pharmacy teams to offer related interventions - for instance weight management services, or the initiation of other evidence-based preventative therapies such as statins in the community setting.
CPS therefore believe that the community pharmacy network should be commissioned to carry out a targeted diabetes screening programme, linking with NHS services to ensure those identified as being at risk are supported to make meaningful lifestyle changes.


























Read our response to the GPhC consultation on draft rules and standards for Responsible and Superintendent Pharmacists, following legislative changes in 2022.