Targeted Diabetes Screening Through Community Pharmacy
Published: 20/11/25

In line with our Manifesto, a key policy area is that of detecting illness in those who may present at the Community Pharmacy with or without symptoms.
It appears that people are accessing the NHS in Scotland later in the course of their illness and more unwell than has been the case in the past.
The reasons for this are many and include:
We are still feeling the impact of the COVID-19 pandemic, where most routine care had to be placed on hold for a significant period of time.
Current waiting times for most services has increased and patients are reportedly struggling to access on-the-day primary care appointments
The Health Foundation has highlighted that there is a link between rising costs of living and people avoiding care services due to financial stress – be that the cost of missing work or transport costs acting as a barrier.
The consequences of this emerging pattern are therefore presenting as:
More critical health events that could be prevented with earlier intervention occurring – for example, heart attacks, strokes and diabetes-related complications.
More advanced cancers at diagnosis, affecting survival rates.
Complex disease at presentation (in particular at Emergency Departments)
Whilst these challenges are not brand new, they have intensified in recent years the world over and as a result the prediction and detection of ill health at the earliest possible stage has become a cornerstone of modern health policy.
We believe that NHS and Scottish Government public health experts should work with CPS to identify screening programmes that the community pharmacy network can support and add value to.
One Such Area Is Targeted Diabetes Screening
The NHS in Scotland spends around £875 million (4.5% of the total budget) annually on diabetes care for almost 340,000 people living with the disease. Over half of this is spent on managing avoidable diabetes-related complications, which are more than twice as likely to occur in people from areas of multiple deprivation. Diagnoses have more than doubled in the last 20 years.
Whilst the ideal scenario would be to prevent diabetes, we should also strive to detect cases of diabetes as early as possible. This can be a challenge as often those unknowingly living with the disease or even the risk of developing it have no reason to engage proactively with the health service.
As such, reaching out into communities with targeted and evidence-based screening programmes should form part of the efforts to reform the NHS and we believe that the community pharmacy network is ideally placed to support this shift in approach.
A recent study using community pharmacy teams in NHS Tayside to identify at-risk individuals and take them through an assessment (and if necessary a point-of-care blood test) has shown that this approach is not only feasible, but more effective than traditional services in terms of use of resources and patient acceptability.
In this study:
46% of those approached to undertake the risk assessment were identified as being at moderate/high risk of developing diabetes. This cohort of people, who would otherwise be unaware of their risk of developing diabetes, were then supported to access advice and care appropriate to their blood test results.
87% were signed up to a digital lifestyle education app
6.2% met the criteria to be referred to an intensive 9-month diabetes prevention programme
6.3% were referred to their GP under suspicion of undiagnosed disease
Whilst these results are in themselves indicative of success, there is huge potential for pharmacy teams to offer related interventions for instance weight management services, or the initiation of other evidence-based preventative therapies such as statins in the community setting.
CPS therefore believe that the community pharmacy network should be commissioned to carry out a targeted diabetes screening programme, linking with NHS services to ensure those identified as being at risk are supported to make meaningful lifestyle changes.
This week’s MCR Ready Reckoner has been updated and is now available to download or you can view it via the App.
An update on March 2026 Part 7 publishing timelines following early finalisation of February adjusted prices. Key dates explained.
PVG membership is now a legal requirement for locum pharmacists in Scotland. Learn what this means and how to apply.
Join Boots Barrhead as a part‑time Pharmacy Technician. Flexible hours, supportive team, checking role, and great benefits.
Join Boots Motherwell as a Pharmacy Technician. Work in a modern, supportive pharmacy with great development and benefits.
Join Boots as a Relief Pharmacist in West Lothian. Enjoy flexible hours, varied locations, strong support, and great benefits.
Join Boots Hamilton as an Independent Prescribing Pharmacist. Shape pharmacy practice with strong team support and great benefits.
Join Boots Largs as a Pharmacy Technician. Work in a supportive store offering Pharmacy First Plus with great benefits and development.
Join Boots Kelso as a Pharmacy Technician. Work in a supportive, community‑focused pharmacy with great benefits and development.
Pharmacy teams will start to notice two new UCF modules appearing in their PMRs from next week - one each for the previously-announced Nystatin and Hydrocortisone PGDs.
Join Boots Glenrothes as an experienced Pharmacist. Work in a high‑performing pharmacy with strong GP links and excellent benefits.
Join Boots Dundee as a Pharmacy Technician. Work in a busy community pharmacy with great support, development, and benefits.
Join Boots Stranraer as a Pharmacist. Work in a well‑supported store with strong leadership, great benefits, and coastal living.
Join Boots Kelso as a Pharmacist. Work in a supportive, community‑focused pharmacy with strong GP links and excellent benefits.
Join Boots Kirkcaldy as a full‑time Pharmacist. Work with a supportive team, deliver excellent care, and enjoy great benefits.
Join Boots Dundee as a Pharmacist. Work with a fantastic team, modern automation, and strong community links with excellent benefits.
Join Boots in Forfar as a Relief Pharmacist. Enjoy flexibility, variety, great benefits, and the chance to make a real community impact.
Join Boots in Oban as an Independent Prescribing Pharmacist. Build your clinical career on Scotland’s west coast with great benefits.
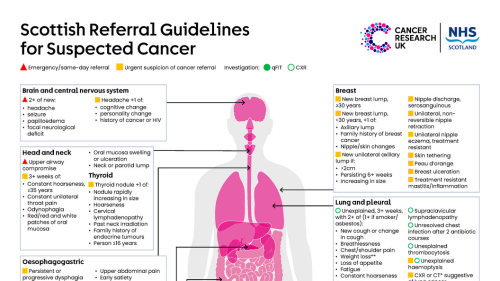
Our colleagues at Cancer Research UK and Healthcare Improvement Scotland have highlighted a useful resource for community pharmacy teams.
Our colleagues at NHS Education for Scotland (NES) have asked us to highlight the Behavioural Change in Healthcare Webinar on Wednesday 18th March 2026 at 7pm.
As of 24 February, the ReThink Dementia campaign is now running. You should have these posters displayed in your pharmacy.
Last Friday, the Community Pharmacy Scotland (CPS) Policy team attended both the Scottish Conservative and Scottish Liberal Democrat party conferences.
Check out our Policy & Development Officer, Gordon Winter, speaking to BBC Radio Scotland yesterday about the shortage of prescription-strength co-codamol.
Learn how the Nip It In The Bud campaign supports early cancer detection in farming and rural communities through awareness and community pharmacy support.
Read our response to the GPhC consultation on draft rules and standards for Responsible and Superintendent Pharmacists, following legislative changes in 2022.
Your next courier collection is scheduled for Thursday, 19th February. We have produced the following guidelines for your prescription bag submissions.
Join Davidsons Chemists in Newburgh, Fife as Pharmacist Manager. Lead a community‑focused team with excellent support, benefits, and development.
Join M&D Green Oban as a Pharmacist Manager. Lead a strong team, support patient care, and enjoy excellent benefits. Apply today.
Join M&D Green Stranraer as a Pharmacist Manager. Lead a great team, develop your career, and enjoy excellent benefits. Apply today.











Guidelines for your prescription courier collection on Thursday, 5th March 2026, including bag usage, required forms and contact details.